Physicians spend nearly 50% of their time on administrative tasks, including documentation in electronic health records (EHRs). Studies show that for every hour spent with patients, doctors spend nearly two hours on documentation. These inefficiencies contribute to physician burnout, reduce patient interaction time, and increase healthcare costs.
Additionally, medical transcription costs healthcare providers an estimated $12 billion annually, while manual documentation errors contribute to misdiagnoses and treatment delays. AI-powered Ambient Digital Scribes offer a revolutionary solution by automating and streamlining clinical documentation.
According to Gartner, ambient AI scribes are set to become integral to EHR workflows, helping alleviate administrative burdens and enhancing care delivery.
AI-Powered Digital Scribes: A Game Changer
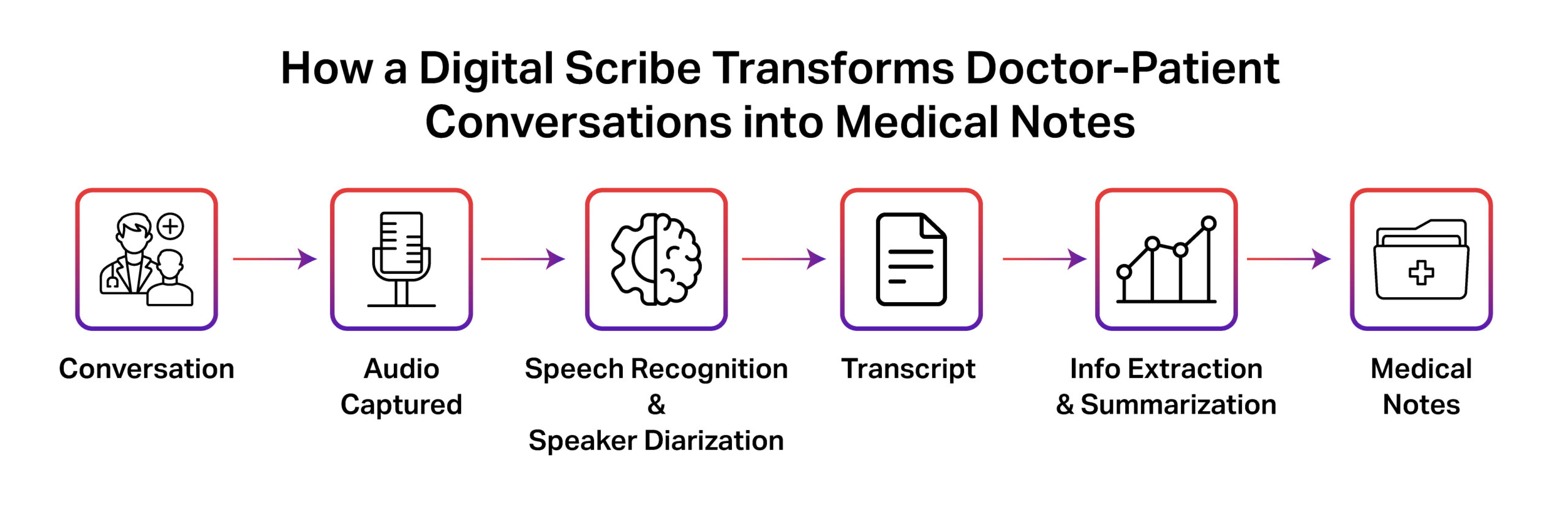
AI-powered Ambient Digital Scribes use Generative AI, Automatic Speech Recognition (ASR), and Natural Language Processing (NLP) to listen, transcribe, and structure doctor-patient conversations in real-time.
Medical Audio Transcription: The Foundation of AI Scribes
Medical audio transcription is the backbone of AI-powered digital scribes, converting spoken medical conversations into structured, actionable text. Traditional transcription services require human intervention, which is not only time-consuming but also prone to inconsistencies. AI-driven transcription solutions have transformed this process using advanced speech-to-text models trained on medical terminology, diverse accents, and contextual nuances.
Key advantages of AI-powered medical transcription include:
- Real-Time Documentation: AI scribes transcribe conversations as they happen, removing the need for post-consultation note-taking.
- Improved Accuracy: AI models recognize complex medical jargon, drug names, and abbreviations with higher precision than manual transcribers.
- Speaker Differentiation: Advanced AI models can distinguish between multiple speakers, doctors, nurses, and patients, ensuring accurate attribution of records.
- Multi-Channel Integration: These systems integrate with dictation tools, telemedicine platforms, and EHRs to streamline end-to-end workflows.
- Scalability: AI-driven transcription reduces dependence on human scribes, enabling healthcare providers to scale services without increasing administrative overhead.
With less time spent on documentation, physicians can focus more on patient care, leading to improved productivity and better patient outcomes.
Benefits for Healthcare Providers
The adoption of AI-driven digital scribes delivers measurable results for healthcare organizations:
- Time Savings: Physicians can reduce documentation time by up to 80%, allowing more time for patient consultations.
- Reduced Costs: Automated documentation brings 30–50% savings in transcription and admin costs.
- Better Patient Care: Improved face-to-face interaction enhances patient satisfaction scores by up to 30%.
- Physician Well-Being: Lower workloads reduce burnout and improve physician retention.
- Fewer Errors: AI scribes reduce documentation errors by up to 60%, minimizing misdiagnoses and communication gaps.
Challenges and Considerations
While AI-powered scribes bring tremendous benefits, there are challenges that healthcare providers must consider:
- Accuracy & Context Understanding: AI models still need training to fully grasp complex medical terminology, patient nuances, and varied accents.
- Data Security & Compliance: Handling sensitive health data demands HIPAA and GDPR-compliant systems with robust encryption.
- Human Oversight: AI-generated notes require physician review to ensure correctness and mitigate liability.
- Audio Capture & Diarization: Noisy clinical settings make it challenging to isolate speech and distinguish between multiple speakers, which impacts transcription accuracy.
- Utterance Segmentation & Context Retention: Medical dialogues are non-linear, and AI models must segment speech while preserving context to ensure coherent documentation.
- Structured Data Extraction: The AI needs to recognize key medical details, such as symptoms, diagnoses, and medications, and understand how they relate to each other to create accurate and organized EHR notes.
- Evaluation Complexity: Beyond word error rate, measuring real-world utility requires clinical benchmarks for entity accuracy, contextual completeness, and HITL validation.
How iMerit Enables AI-Powered Scribing
Developing high-performing AI scribes requires high-quality annotated medical datasets. iMerit specializes in medical data annotation, including medical transcription labeling, NLP dataset curation, and structured EHR documentation training. iMerit’s domain expertise ensures that AI models are trained on accurate, real-world datasets that improve automation and clinical decision-making.
With deep expertise in speech-to-text AI, audio segmentation, and domain-specific transcription annotation, iMerit helps healthcare AI companies build more accurate and reliable digital scribes. By providing high-quality labeled data, iMerit ensures that AI models can handle real-world clinical environments with precision.
Why Choose iMerit?
- Comprehensive Data Annotation: Precisely labeled medical datasets ensure AI-powered scribes capture and process clinical conversations accurately.
- Domain-Specific AI Training: Our teams work across various medical specialties, from oncology to orthopedics, enabling deep understanding of complex terminology.
- Scalable AI Solutions: We provide end-to-end annotation and model training services to support large-scale healthcare deployments.
- Security & Compliance: We follow strict HIPAA and GDPR compliance to protect patient confidentiality.
- Integrated Annotation Platform: iMerit’s Ango Hub is purpose-built for medical AI workflows. It supports audio transcription labeling, speaker diarization, utterance segmentation, and structured data extraction. With built-in QA workflows and collaboration tools, Ango Hub ensures high-quality, consistent annotations that accelerate the development of reliable digital scribes.
Ready to streamline clinical documentation with next-gen AI scribes? Partner with iMerit to accelerate your AI healthcare solutions.
What does the Future hold
The adoption of AI-powered Ambient Digital Scribes is rapidly growing. By 2026, the global AI healthcare market is expected to reach $67 billion, with AI-driven medical documentation playing a key role. Leading hospitals and healthcare providers are integrating AI scribes to improve efficiency, reduce costs, and enhance care quality.
Future advancements in AI-powered scribes include:
- Multimodal AI: Combining voice, text, and image inputs to generate rich, context-aware patient records.
- Predictive Analytics: Transcriptions enriched with AI that identify early signs of disease and suggest treatment options.
- Real-Time Summarization: Instant summaries of visits, along with follow-up recommendations based on medical history.
- Multilingual & Specialty-Specific Scribes: Support for multiple languages (e.g., Spanish, Mandarin) and specialized fields like cardiology or oncology improves accessibility and accuracy.
As AI technology continues to evolve, digital scribes will become even more intelligent and adaptable. The future of AI-driven healthcare documentation lies in deeper contextual understanding, enhanced data security, and broader integration with healthcare systems.
According to a Gartner use-case comparison, automating EHR documentation is among the top “Likely Wins” for healthcare providers adopting GenAI, due to its high value and feasibility across clinical workflows.
Recap: What These Solutions Deliver
AI-powered digital scribes offer a transformative edge for healthcare by:
- Automatically transcribing patient interactions with up to 98% accuracy.
- Extracting key medical details, including symptoms, diagnoses, and treatments, in real time.
- Integrating seamlessly with EHR systems, reducing manual entry time by up to 80%.
- Ensuring HIPAA-compliant handling of sensitive data for secure and ethical deployment.
By minimizing documentation time, physicians can redirect their focus to patient care, enhancing productivity, satisfaction, and clinical outcomes.
