Utilization Management for Claims Processing
iMerit improved this healthcare insurance provider’s claims processing model using Ango Hub’s natural language processing and computer vision technology.
Challenge
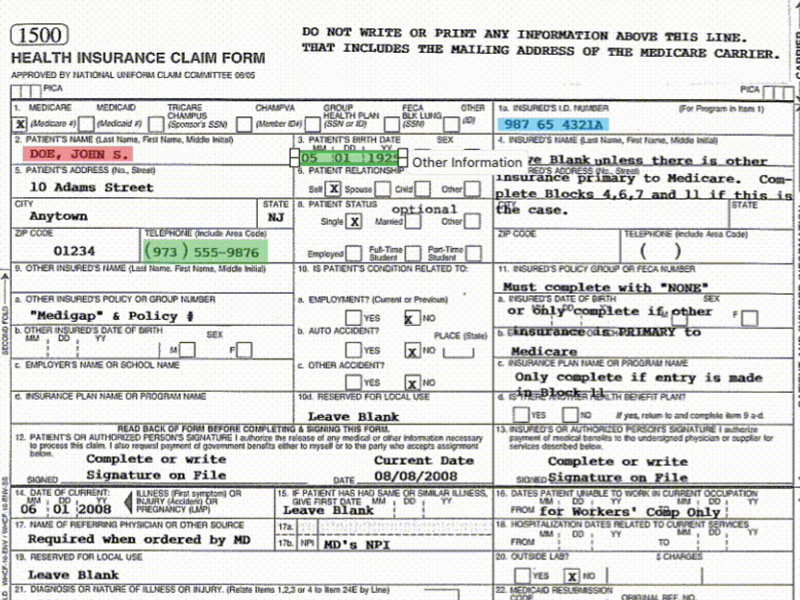
Each day, healthcare insurance providers receive millions of documents from offices, hospitals, and other insurance providers. Historically, these health records are received, compiled, and processed by humans. After costs began mounting from falsely declined claims, this top healthcare insurance provider realized it needed document AI to help extract and summarize the complex information in medical records. As documents were becoming increasingly non-standardized, computer vision and natural language processing technologies were becoming essential to processing claim efficiently.
This original process was creating delays in claims processing, as well as poorer resulting data extraction. Due to the rapidly increasing volume and complexity of incoming information, this company realized it needed to boost the performance of its model to prevent further turmoil.
“Audits were costing us. Improving the output of our models stood to change how we saw our business. ”
- Director, Data Science & AI
Solution
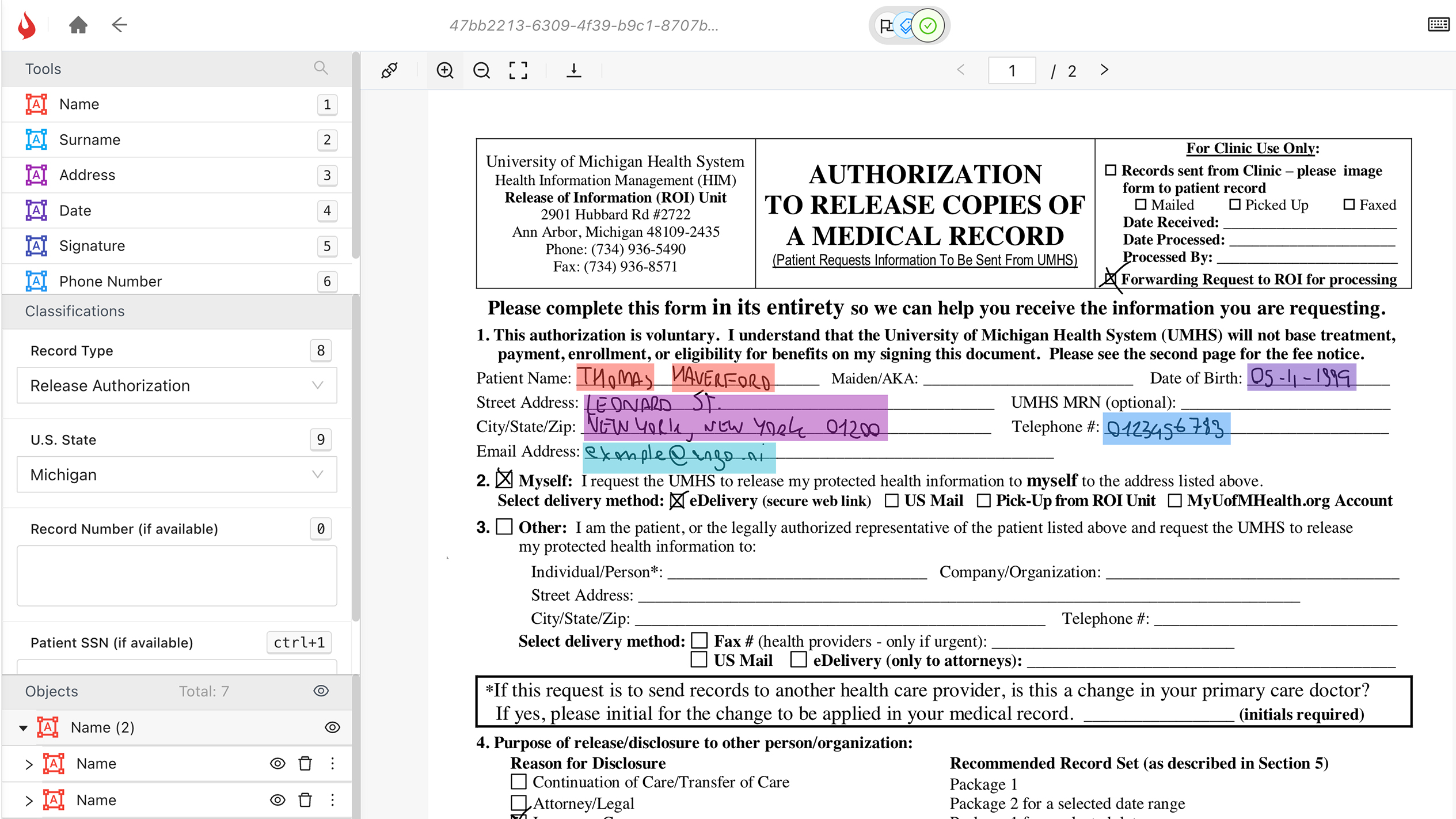
After a brief consultation, iMerit proposed its Ango Hub solution which uses computer vision to localize information within PDFs and natural language processing functionality with optical character recognition to classify, link, and extract data. iMerit’s teams then generated data to tune a foundational Large Language Model to perform summarization.
To begin, iMerit created links to the data servers, maintaining HIPPA and data governance on our client’s servers. Specialized healthcare annotators and a customized workflows was then applied that adhered to regulatory standards. Batches of medical data were given to these annotators featuring sensitive information like patient and provider names, insurance numbers, member IDs, group numbers, diagnoses, diagnostic codes, procedures codes, CPT codes, ICD-10 xcodes.
Using Ango Hub to annotate the data, the specialized healthcare annotators were able to extract the data and create training datasets to begin training a new model.

Result
Once iMerit trained this company’s computer vision and natural language processing algorithms, claims processing time not only became more accurate, but also more efficient. The resulting model’s efficiency accelerated claims processing time by 24%, with a 68% reduction in manual audits. Within six months, these performance improvements saved this company an estimated $180M, owing to increased customer satisfaction and reduced staffing for quality assurance audits.